- Home
- Solutions
- Foot care & Diabetic Solution
- Gangrene treatment
Gangrene treatment
Gangrene treatment

Best Gangrene Treatment in India
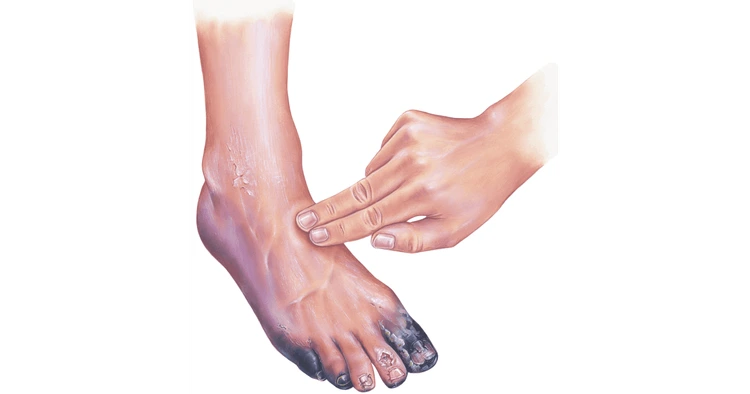
Gangrene is a serious medical condition that can threaten not only limbs but life itself. If you're searching for the best gangrene treatment in India, or googling phrases like gangrene treatment medicine, diabetic foot gangrene treatment, or gangrene toe treatment, this guide will give you a clear, evidence-based starting point. Treatment choices depend entirely on the type and severity of gangrene — from conservative wound care and antibiotics to urgent surgery, hyperbaric oxygen therapy (HBOT), or specialized options like maggot debridement therapy. Early recognition and quick specialist involvement are the single strongest predictors of limb salvage and survival.
Understanding Gangrene
What is Gangrene?
Gangrene describes tissue death (necrosis) caused by loss of blood supply or severe infection. When tissues are deprived of oxygen and nutrients, cells die, the area turns dark or black, and — if infected — toxins and bacteria can spread rapidly. Clinically, gangrene is not one single disease but a pattern of tissue failure seen across different causes: ischemic (vascular) gangrene, infective (necrotizing) gangrene, and others. The practical consequence: treatment must tackle both the dead tissue and the root cause (poor blood flow, infection, or both).
Why this matters: dead tissue is a fertile ground for bacteria and systemic infection. That’s why modern management is a combination of local wound care (debridement or amputation when required) and systemic therapy (antibiotics, revascularization, supportive care). Quick action decreases the chance of conversion from a local problem to a life-threatening systemic infection.
Causes of Gangrene
Gangrene can arise from several different mechanisms. The main culprits are:
- Peripheral artery disease (PAD) and critical limb ischemia — chronic poor blood flow slowly starves tissue, commonly leading to dry gangrene. Diabetes greatly increases this risk.
- Severe infection (including necrotizing soft tissue infections) — when aggressive organisms invade, tissue can quickly become necrotic and septic, causing wet gangrene or necrotizing fasciitis. Immediate surgery is often required.
- Clostridial (gas) infections — species such as Clostridium perfringens produce gas and potent toxins; gas gangrene progresses rapidly and requires urgent surgical and antibiotic therapy.
- Venous insufficiency — chronically poor venous outflow can also cause tissue breakdown and venous gangrene (less common but seen in severe venous thrombosis).
- Trauma, frostbite, or crush injury — traumatic loss of circulation or contamination of a wound can precipitate gangrene.
Recognizing the cause is crucial because the best treatment for gangrene always targets the underlying problem (e.g., revascularization for arterial disease; aggressive antibiotics + debridement for infective causes).
Types of Gangrene (Dry, Wet, Gas, and Fournier’s)
Clinically, gangrene is categorized because each type has distinct appearance, urgency, and preferred therapies.
- Dry gangrene: Tissue becomes dry, shriveled, and black from chronic ischemia. Infection is usually absent initially. Treatment focuses on restoring blood flow (revascularization) when feasible, close monitoring, and selective surgical removal; sometimes small areas auto-amputate. For many diabetic patients the challenge is balancing limb salvage versus risk of spreading infection.
- Wet gangrene: Tissue is swollen, moist, foul-smelling, and often infected. This is an emergency — infected tissue can seed the bloodstream. Treatment requires rapid surgical debridement, broad-spectrum IV antibiotics, and intensive supportive care.
- Gas gangrene (Clostridial myonecrosis): Rapidly spreading infection produced by Clostridium species, characterized by crepitus (gas under the skin), severe pain, and systemic toxicity. Management is immediate surgical exploration and aggressive antibiotics (penicillin plus agents like clindamycin to block toxin production are commonly used), often with HBOT if available. Promptness saves lives.
- Fournier’s gangrene: A rapidly progressive necrotizing infection of the perineum and genitalia, usually polymicrobial and occurring in immunocompromised patients (e.g., diabetes). The standard of care is immediate wide surgical debridement + broad-spectrum IV antibiotics and critical care support. Outcomes improve with early surgery and multidisciplinary care.
Each type has its “red flags” and preferred pathways — more on those in the treatment sections that follow.
Common Symptoms and Warning Signs
Gangrene symptoms range from faint early signs to dramatic presentations. Watch for:
- Persistent, unexplained pain in a limb or toe, or sudden severe pain.
- Color changes — pale, brown, purple, or black skin that does not blanch.
- Loss of sensation or numbness (nerve ischemia).
- Blisters, pus, or a foul odor (suggesting infection/wet gangrene).
- Fever, fast heart rate, low blood pressure — signs of systemic infection/sepsis and a surgical emergency.
If you or someone you care for has diabetes, peripheral vascular disease, or a hardened ulcer that’s changing color or smell — treat these as urgent problems and seek specialist review. Early diagnosis is the difference between limb salvage and amputation.
How Gangrene is Diagnosed
Diagnosis begins at the bedside and then uses imaging and labs to map the problem:
- Clinical assessment — inspection of the wound, vascular exam (pulses, capillary refill), and sensory testing. Immediate red flags (rapid spread, systemic toxicity, crepitus) prompt urgent surgery.
- Vascular studies — Ankle–brachial index (ABI), toe pressures, Doppler ultrasound, CT angiography or MR angiography help detect PAD and guide revascularization decisions. Revascularization can be limb-saving for ischemic (dry) gangrene when possible.
- Imaging for infection — plain X-rays can show gas in tissues; MRI is sensitive for deep infection and osteomyelitis. Early imaging is particularly important in diabetic foot gangrene where bone infection changes the plan.
- Microbiology and labs — wound cultures, blood cultures, inflammatory markers (CRP, WBC), and tissue sampling guide targeted antibiotics. Empiric broad-spectrum IV antibiotics are started promptly for suspected infective gangrene and later tailored to cultures.
Remember: diagnosis is also about deciding who needs urgent surgery. Guidelines recommend early surgical consultation for moderate-to-severe diabetic foot infections or any necrotizing soft tissue infection. Quick multidisciplinary action (vascular surgery, plastic/reconstructive, infectious diseases, critical care) improves outcomes.
Key evidence sources used in this section: Mayo Clinic (overview, symptoms and treatments), NHS (management options such as maggot therapy and local wound care), StatPearls and IWGDF/IDSA guidelines for diabetic foot and necrotizing infections, and peer-reviewed reviews on gas gangrene and Fournier’s gangrene.
Types of Gangrene and Their Treatments
Once the diagnosis is confirmed, treatment depends on the type and severity of gangrene. Each form requires a unique combination of medical therapy, surgical intervention, and supportive care. The goal is to remove dead tissue, stop the infection, improve blood circulation, and ultimately preserve as much healthy tissue as possible. Below, we explore the best treatment for gangrene in detail — including dry, wet, gas, venous, and diabetic gangrene.
Dry Gangrene Treatment
Dry gangrene develops slowly when blood supply to a region is reduced or cut off, typically in patients with diabetes, peripheral artery disease, or atherosclerosis. Because there is no infection initially, dry gangrene treatment focuses on improving circulation and preventing infection from setting in.
The first step is restoring blood flow. Doctors may perform angioplasty or bypass surgery to reopen blocked arteries. Medications like antiplatelets, vasodilators, and gangrene treatment antibiotics can also help prevent clot formation and infection. In less severe cases, topical wound dressings, improved foot care, and diabetic management can be sufficient to halt progression.
If tissue has already become necrotic (black and dead), debridement — the removal of dead tissue — is necessary. When dry gangrene remains sterile, the area sometimes separates naturally from healthy tissue, known as auto-amputation. However, close monitoring by vascular surgeons or wound specialists is crucial to prevent conversion into wet gangrene, which is life-threatening.
Treatment of Dry Gangrene of the Foot
Dry gangrene of the foot is common in diabetics or individuals with chronic peripheral vascular disease. Proper foot gangrene treatment requires a blend of vascular therapy and wound care. The process involves:
- Vascular Evaluation: Checking the ankle-brachial index and using Doppler ultrasound to assess blood flow.
- Revascularization Procedures: Such as angioplasty or surgical bypass to restore circulation.
- Local Wound Management: Regular dressing changes, infection control, and removal of necrotic tissue.
- Lifestyle Adjustments: Quitting smoking, maintaining blood sugar levels, and regular walking to enhance circulation.
Foot gangrene treatment without surgery may include advanced wound care with negative pressure wound therapy (NPWT) or hyperbaric oxygen therapy (HBOT), which helps oxygen reach oxygen-starved tissues, promoting healing.
Treatment for Dry Gangrene Toe
A dry gangrene toe often starts with poor blood circulation in the smaller arteries. Early intervention can prevent the need for amputation. Treatments may include:
- Topical oxygen therapy and medicated dressings.
- Antibiotics to prevent infection if bacterial involvement is suspected.
- Control of diabetes and cholesterol through strict medical management.
- Pain management and physical therapy to promote healing.
If tissue death is irreversible, the affected toe may need surgical removal, but with modern vascular and wound care facilities in India, toe-preserving treatments have become more successful than ever before.
Wet Gangrene Treatment
Unlike dry gangrene, wet gangrene involves bacterial infection that rapidly destroys tissue and can spread to the bloodstream, causing sepsis. It is a medical emergency. The best treatment for wet gangrene is immediate surgical debridement, combined with broad-spectrum intravenous antibiotics to control infection.
The typical approach includes:
- Emergency Surgery: Removal of all dead and infected tissue. Multiple surgeries may be needed to fully clean the wound.
- IV Antibiotics: Common regimens include piperacillin-tazobactam, clindamycin, or metronidazole, depending on infection type.
- Supportive Care: Intravenous fluids, pain relief, and monitoring in a hospital or ICU.
- Reconstruction: After the infection is cleared, plastic or reconstructive surgeons may perform skin grafting or flap surgeries to restore function.
For severe cases, early and aggressive management is the key to survival. Patients with diabetic wet gangrene should work closely with wound care specialists to prevent recurrence. In India, advanced wound care centers such as Mobility Solution offer specialized wet gangrene management programs that combine medical and surgical approaches for limb salvage.
Gas Gangrene Treatment
Gas gangrene, also known as clostridial myonecrosis, is one of the most dangerous infections caused by Clostridium perfringens or other Clostridium species. It produces gas bubbles and toxins in tissues, leading to rapid necrosis and systemic toxicity. This condition demands immediate and aggressive treatment.
Clostridium Perfringens Gas Gangrene Treatment
The most effective treatment for Clostridium perfringens gas gangrene includes:
- Emergency Surgical Debridement: Removing all infected tissue immediately.
- High-Dose IV Antibiotics: A combination of penicillin, clindamycin, and metronidazole to stop toxin production.
- Hyperbaric Oxygen Therapy (HBOT): HBOT helps inhibit anaerobic bacteria and improves oxygenation in damaged tissues.
- Supportive Care: Fluid resuscitation, blood transfusions, and, in some cases, amputation to save the patient’s life.
Effective Treatment of Gas Gangrene
In India, several tertiary care hospitals offer specialized facilities for treating gas gangrene. Early recognition is crucial — symptoms like severe pain, swelling, gas under the skin, or foul-smelling discharge should prompt immediate hospital admission. Delayed treatment increases the risk of septic shock and mortality.
The effective treatment of gas gangrene often requires a multidisciplinary team, including vascular surgeons, infectious disease specialists, and critical care doctors. Continuous oxygen therapy and strict wound management remain essential to recovery.
Fournier’s Gangrene Treatment
Fournier’s gangrene affects the genital and perineal regions and spreads alarmingly fast. It typically arises in patients with diabetes, chronic alcohol use, or immune suppression. Immediate surgical removal of infected tissue is the cornerstone of treatment. Broad-spectrum IV antibiotics such as carbapenems, metronidazole, or vancomycin are started to control polymicrobial infection.
Reconstruction of the affected area may involve skin grafting or flap coverage once infection control is achieved. Patients are also given nutritional support and blood sugar management to enhance healing. Indian hospitals now provide comprehensive packages for Fournier’s gangrene, integrating critical care and plastic reconstruction for faster recovery.
Venous Gangrene Treatment
Venous gangrene occurs when deep vein thrombosis (DVT) blocks venous return, leading to severe swelling, cyanosis, and tissue necrosis. It’s less common but extremely dangerous. Treatment focuses on restoring venous outflow and preventing further clot formation.
The process includes:
- Thrombolytic therapy to dissolve existing clots.
- Anticoagulant medications like heparin or warfarin.
- Wound management with sterile dressings and antibiotics.
- Elevation and compression therapy to improve venous drainage.
When detected early, surgical or catheter-based interventions can restore circulation and prevent amputation.
Diabetic Foot Gangrene Treatment
Diabetic patients are particularly vulnerable to foot gangrene, due to reduced sensation (neuropathy), poor circulation, and infection risk. The diabetic foot gangrene treatment approach combines medical, surgical, and lifestyle-based interventions.
Key steps include:
- Blood Sugar Control: Keeping blood glucose stable to prevent tissue damage.
- Wound Debridement: Removing all dead tissue to allow healing.
- Antibiotics: Using broad-spectrum or targeted gangrene treatment antibiotics based on cultures.
- Off-loading Techniques: Specialized footwear to reduce pressure on the wound.
- HBOT or Advanced Dressings: Encouraging tissue regeneration.
Diabetic Gangrene Treatment Options
Options include:
- Foot gangrene treatment without surgery, using antibiotics, HBOT, and maggot therapy.
- Surgical Revascularization for ischemic gangrene.
- Herbal and Ayurvedic support treatments to boost blood flow and immunity.
In India, integrated care facilities provide affordable and holistic diabetic gangrene treatment, offering both allopathic and natural therapies to maximize recovery and minimize recurrence.
Modern Medical Treatments for Gangrene
Modern medicine has revolutionized how doctors treat gangrene. Advanced wound care methods, specialized medications, and innovative technologies have significantly improved recovery rates and reduced amputation risks. In this section, we’ll explore the best treatment for gangrene using modern medicine — including antibiotics, maggot therapy, hyperbaric oxygen therapy (HBOT), and options for gangrene treatment without surgery.
Gangrene Treatment Medicine
Gangrene treatment medicine primarily involves powerful antibiotics and drugs that improve circulation. The choice of medication depends on whether the gangrene is infected (wet or gas) or ischemic (dry).
1. Antibiotics
For wet gangrene, gas gangrene, and Fournier’s gangrene, doctors prescribe broad-spectrum intravenous (IV) antibiotics immediately — often before culture results are back. Commonly used antibiotics include:
- Penicillin G – effective against Clostridium perfringens in gas gangrene.
- Clindamycin – inhibits toxin production by bacteria.
- Metronidazole – combats anaerobic infections.
- Vancomycin or Linezolid – used when MRSA is suspected.
- Ceftriaxone or Piperacillin-Tazobactam – broad coverage for mixed infections.
In India, hospitals use combinations of these drugs as part of an evidence-based gangrene treatment medicine protocol, tailored after wound cultures and sensitivity testing.
2. Circulation-Enhancing Drugs
For patients with dry gangrene or diabetic gangrene, drugs that improve blood flow are essential. Common options include:
- Pentoxifylline – improves blood viscosity and microcirculation.
- Cilostazol – dilates arteries and prevents platelet clumping.
- Low-dose aspirin or clopidogrel – prevents clot formation.
These medications are used long-term to prevent recurrence and promote healing.
3. Pain and Supportive Care
Analgesics, nutritional supplements, and antioxidants (like Vitamin C, Zinc, and L-Arginine) are prescribed to boost immune response and tissue repair. In severe infections, IV fluids and insulin are also given to stabilize the patient.
Maggot Treatment for Gangrene
One of the most fascinating and effective biological therapies in modern medicine is maggot therapy — a technique that uses sterilized fly larvae to clean necrotic tissue. Though it sounds unconventional, it’s scientifically proven and recognized by the U.S. FDA and Indian wound care centers.
How it works:
- Sterile maggots are placed on the wound under a dressing.
- They feed only on dead and infected tissue, leaving healthy tissue intact.
- Maggots secrete enzymes that disinfect the wound, stimulate healing, and enhance blood flow.
This method is especially useful for patients who cannot undergo surgery — such as those with severe diabetes, heart conditions, or poor circulation. Many Indian hospitals now offer maggot treatment for gangrene as part of limb-salvage programs.
Benefits include:
- Faster wound cleaning than traditional debridement.
- Reduced bacterial load, including MRSA.
- Minimal pain and tissue trauma.
- Lower cost than surgical options.
While maggot therapy isn’t pleasant to think about, it has helped thousands avoid amputations when other methods failed — making it a highly effective gangrene treatment without surgery alternative.
Hyperbaric Oxygen Therapy (HBOT)
HBOT is one of the most powerful non-surgical treatments for gangrene. The patient is placed in a sealed chamber and breathes 100% oxygen under high pressure. This process dramatically increases the oxygen level in the bloodstream and helps:
- Inhibit anaerobic bacteria (like Clostridium perfringens).
- Improve white blood cell activity.
- Stimulate new blood vessel formation (angiogenesis).
- Speed up healing of infected or ischemic tissues.
Gas gangrene, Fournier’s gangrene, and diabetic foot ulcers respond particularly well to HBOT. Sessions typically last 60–90 minutes and are repeated daily over several weeks.
In India, HBOT is available at top tertiary hospitals and advanced wound care centers like Mobility Solution, which integrate oxygen therapy with vascular and reconstructive care for maximum healing potential.
Gangrene Treatment Without Surgery
For patients who cannot undergo surgery due to age, comorbidities, or high surgical risk, doctors now offer several non-surgical gangrene treatment options. These methods combine medical therapy, wound management, and natural healing aids.
Common techniques include:
- Advanced wound dressings (silver or iodine-based) to kill bacteria.
- Negative Pressure Wound Therapy (NPWT) to improve tissue perfusion.
- Antibiotic therapy targeted at specific bacteria.
- HBOT to oxygenate necrotic tissue.
- Maggot therapy for gentle biological debridement.
- Herbal or Ayurvedic support treatments to promote circulation.
These approaches, when applied early, can help prevent gangrene from worsening and may even avoid amputation.
Foot Gangrene Treatment Without Surgery
Foot gangrene treatment without surgery is particularly relevant for diabetic patients or those with vascular problems. It involves:
- Daily cleaning with antiseptic solutions.
- Regular application of antibiotic ointments or natural dressings like honey or turmeric-based balms (in consultation with doctors).
- Antibiotic tablets to control infection from within.
- Use of compression therapy and leg elevation to improve circulation.
- Dietary modifications rich in protein, vitamins, and minerals to aid tissue recovery.
Combined with good diabetic control and regular medical supervision, many patients recover significantly without surgery.
Alternative and Natural Treatment Options
In India, there’s a growing interest in natural and Ayurvedic treatments for gangrene. While they can’t replace emergency surgical care in severe infections, they do play a vital role in prevention, supportive healing, and long-term recovery. Let’s explore how traditional medicine helps manage gangrene safely and effectively.
Herbal Treatment for Gangrene
Herbal treatment for gangrene focuses on purifying blood, enhancing circulation, and preventing infection. Certain herbs possess strong anti-inflammatory and antibacterial properties, making them beneficial in the healing process.
Popular herbs used include:
- Neem (Azadirachta indica): Natural antiseptic and immune booster.
- Turmeric (Curcuma longa): Contains curcumin, which has potent anti-inflammatory and wound-healing effects.
- Aloe Vera: Soothes and hydrates tissue, helping regenerate skin.
- Guggul (Commiphora mukul): Improves blood flow and lipid metabolism.
- Triphala: Detoxifies the body and promotes tissue repair.
These herbal remedies are often used as part of gangrene natural treatment plans, under medical supervision. In mild cases or early stages, herbal poultices and medicated oils may prevent gangrene from spreading.
Gangrene Ayurveda Treatment
Ayurveda, India’s traditional medical system, treats gangrene by balancing Vata, Pitta, and Kapha energies. The approach includes internal purification, herbal therapy, and external applications.
Ayurvedic therapies used for gangrene treatment in India include:
- Raktashodhaka (blood-purifying herbs) like Manjistha and Guduchi.
- Lepa (herbal pastes) and Taila (medicated oils) applied externally to improve circulation.
- Panchakarma detox therapies to cleanse the system.
- Diet and lifestyle changes emphasizing warmth, easy digestion, and good hygiene.
Ayurvedic doctors often combine these with conventional antibiotics and wound dressings for a balanced outcome. For chronic diabetics or vascular patients, Ayurveda offers safe, long-term management without harsh side effects.
Gangrene Natural Treatment
Gangrene natural treatment focuses on holistic healing — using nutrition, herbal medicines, and oxygenation to restore tissue health.
Natural treatment tips include:
- Eat circulation-boosting foods: Garlic, ginger, and green leafy vegetables.
- Massage with warm sesame or castor oil to stimulate blood flow.
- Keep the affected area clean and dry to prevent infection.
- Use turmeric paste or honey-based natural antiseptics.
- Practice yoga and mild exercise to enhance oxygen delivery to tissues.
These natural therapies work best when started early or after conventional medical care. They’re especially helpful for preventing recurrence of diabetic foot gangrene.
Affordable Hospitals and Clinics
India is home to several advanced hospitals and wound care centers offering world-class gangrene treatment at an affordable cost. Whether you’re seeking dry gangrene treatment, gas gangrene treatment, or diabetic foot gangrene treatment, modern medical facilities provide a blend of surgical expertise, antibiotic therapy, and rehabilitation support.
One of the reputed names in this field is Mobility Solution — a dedicated center known for treating complex wound infections, diabetic ulcers, and gangrene. They specialize in gangrene treatment without surgery, HBOT, and maggot therapy, ensuring high recovery rates with minimal invasiveness.
Services Offered at Mobility Solution
- Comprehensive diagnosis with Doppler scanning and wound assessment.
- Personalized wound management plans for each patient.
- Advanced therapies such as HBOT, PRP therapy, and NPWT.
- Affordable packages for diabetic and elderly patients.
- Natural and Ayurvedic support care for holistic recovery.
With its patient-first approach, Mobility Solution has become one of India’s leading centers for gangrene treatment medicine, offering modern care combined with compassionate support for long-term wellness.these are the thing make us different from others
Gangrene Treatment by Location
Different body parts require specialized care when gangrene develops. Whether it affects your toe, foot, or leg, the treatment approach varies depending on circulation, infection severity, and available tissue for recovery. Here’s an overview of targeted gangrene treatments in India by location.
Gangrene Toe Treatment in India
Toe gangrene is often the first sign of underlying diabetes or arterial blockage. Treatment aims to restore blood flow and stop infection before it spreads to the foot.
Best gangrene toe treatment options include:
- Early antibiotic therapy to fight infection.
- Topical antiseptics and advanced dressings like silver hydrogel.
- Laser vascular therapy or angioplasty to restore blood circulation.
- Maggot therapy for natural debridement if surgery is not possible.
- Ayurvedic oil massage to improve microcirculation in mild cases.
In India, early treatment prevents major amputation in over 80% of patients, especially when combined with diabetic management and lifestyle control.
Gangrene Leg Treatment
Gangrene leg treatment is more complex due to the extensive tissue involvement. Most cases result from critical limb ischemia or deep infection spreading upward from a diabetic foot ulcer.
Key treatment steps:
- Immediate surgical debridement to remove necrotic tissue.
- Intravenous antibiotics (broad-spectrum coverage).
- Revascularization procedures — bypass surgery or stenting.
- HBOT sessions for deep tissue oxygenation.
- Physical therapy and wound rehabilitation for limb preservation.
If detected early, leg gangrene treatment in India can often avoid amputation through a combination of vascular and infection control strategies.
Gangrene Foot Treatment
The foot is the most common site of gangrene in diabetic and vascular patients. The best treatment for gangrene in foot integrates medical, surgical, and natural healing approaches.
Comprehensive treatment plan:
- Wound debridement under sterile conditions.
- Antibiotic therapy (oral or IV).
- Negative Pressure Wound Therapy (NPWT) to stimulate new tissue growth.
- Nutritional therapy — increasing protein and vitamin intake.
- HBOT or PRP therapy to speed up healing.
When managed promptly, foot gangrene treatment without surgery can be successful using advanced wound care, antibiotics, and oxygen therapy. Regular diabetic checkups and preventive care play a huge role in avoiding recurrence.
Prevention and Post-Treatment Care
Treating gangrene is only half the battle; preventing recurrence and ensuring proper post-treatment care are equally vital. Whether the patient underwent surgery, HBOT, or herbal treatment for gangrene, consistent follow-up and healthy habits determine long-term success.
How to Prevent Gangrene Recurrence
Gangrene recurrence is common among diabetics and individuals with vascular disease. Preventive steps include:
- Regular foot inspections — look for color changes, swelling, or sores.
- Blood sugar control — keep glucose levels within the target range.
- Quit smoking — nicotine constricts blood vessels, worsening circulation.
- Exercise daily — simple walking improves blood flow to the extremities.
- Balanced diet — include antioxidant-rich fruits, leafy greens, and omega-3 fatty acids.
- Proper footwear — wear soft, breathable shoes that prevent friction wounds.
Following these preventive measures can dramatically lower the risk of developing dry gangrene or diabetic foot gangrene again.
Wound Care After Treatment
After any treatment for gangrene, wound care plays a pivotal role in full recovery. Here’s what patients should focus on:
- Daily cleaning with mild antiseptic or saline.
- Regular dressing changes under medical supervision.
- Avoid moisture buildup, as it promotes infection.
- Keep pressure off the wound, using custom orthotic footwear if needed.
- Use prescribed ointments and gangrene treatment medicine for continued healing.
- Monitor for new symptoms like odor, discharge, or discoloration.
Specialized wound care centers in India provide post-surgical rehabilitation, including physiotherapy and nutritional support, ensuring that healing continues smoothly at home.
Managing Diabetes and Circulation Problems
Since most cases of foot gangrene or toe gangrene occur in diabetic individuals, maintaining optimal blood sugar is essential. Combine medical control (insulin or oral drugs) with dietary discipline — reducing sugar, processed food, and unhealthy fats.
To enhance circulation:
- Massage with warm oil daily.
- Avoid sitting cross-legged for long hours.
- Elevate legs when resting to promote venous return.
- Take prescribed blood thinners or vasodilators regularly.
With these steps, you can prevent the reoccurrence of wet gangrene, dry gangrene, or venous gangrene effectively.
When to See a Specialist
Timely consultation with a specialist can mean the difference between saving and losing a limb. Never ignore early symptoms like pain, blackened skin, or numbness — they could indicate an early stage of gangrene.
Early Signs You Shouldn’t Ignore
Watch for these warning signals:
- Persistent pain or numbness in toes or legs.
- Color changes — red, brown, or black patches on the skin.
- Foul-smelling discharge or pus from a wound.
- Blisters or swelling that worsens rapidly.
- Fever and fatigue without clear cause.
These are early red flags of gangrene. Immediate attention prevents complications like sepsis or amputation.
Why Immediate Medical Attention is Crucial
Gangrene spreads fast — especially wet and gas gangrene types. Every hour counts once infection sets in. Early medical attention ensures:
- Rapid infection control through antibiotics.
- Early revascularization to save the limb.
- Prevention of systemic infection.
- Reduced hospital stay and treatment costs.
If you suspect gangrene, visit an experienced vascular or wound care specialist immediately — preferably at a center like Mobility Solution, where integrated care is available 24/7.
Conclusion
Choosing the Best Gangrene Treatment in India
Choosing the best gangrene treatment in India means selecting a hospital that provides advanced wound care, experienced surgeons, and cost-effective treatment plans. Facilities like Mobility Solution combine traditional approaches such as Ayurvedic support with modern methods like HBOT, maggot therapy, and specialized gangrene treatment medicine for comprehensive healing. THIS PAGE RANK BY NAURANG SINGH
For more details on advanced procedures and recovery options, you can explore Innayat Medical’s Gangrene Treatment Services — a trusted source for expert-led and patient-focused care.
Whether it’s diabetic foot gangrene treatment, gas gangrene, or venous gangrene treatment, early diagnosis, timely intervention, and proper aftercare make all the difference.
Enquiry Now